Compare your options & be empowered
What care is right for you?
Most people delay surgery as long as possible, especially with spinal fusion, due to risks like adjacent segment breakdown and potential reoperation. However, conservative care options—such as lifestyle changes, medications, and chiropractic treatments—can be effective early on. When non-surgical methods fail to provide relief, motion surgery offers an innovative solution, allowing patients to seek care earlier without the downsides of fusion. This is procedural innovation, giving you more choices for long-term mobility and relief.

Endoscopic Decompression
Endoscopy of the spine follows the use of endoscopes in other joints of the musculoskeletal system, including knee, hip, shoulder, ankle, and wrist. The main purpose of using endoscopic technology and techniques is to create the smallest amount of tissue trauma to resolve a given pathology, normally without the use of supplemental instrumentation. Endoscopic spine surgery is currently the least invasive of all so-called minimally invasive surgery (MIS) techniques.
Development of percutaneous (needle-based) spine treatments started in the 1960s with the contributions of Dr. Lyman Smith, who treated disc-related pathology with chymopapain. In the 1970s Dr. Hijikata published the first reports of percutaneous nucleotomy in Japan, followed by Dr. Parviz Kambin in the 1980s who described a safe working passage known today as Kambin’s triangle. Kambin’s procedure later became known as the lateral extraforaminal approach, utilizing small diameter scopes for direct vision of disc pathology aided by high-intensity light and water irrigation. Endoscopic spine technology as we know it today was generally developed by Dr. Anthony Yeung. Dr. Yeung was the first to utilize endoscopic approaches for surgical correction of both soft and hard tissue pathology of the lumbar spine.
Endoscopic decompression is considered the least invasive motion preserving surgery, allowing decompression of neural elements while creating the smallest possible amount of additional spinal instability. Some benefits associated with endoscopic decompression include diminished soft tissue collateral damage, minimal blood loss, and direct visualization of neural structures. Most endoscopic surgeries are performed as out-patient procedures, often with sedation rather than using general anesthesia. Spine conditions often treated with endoscopic surgery include disc herniation, spinal stenosis, cyst removal, and nerve ablation or nerve transection.
Currently there are several companies in the United States offering technology for endoscopic spine care including:
Cervical Disc Replacements
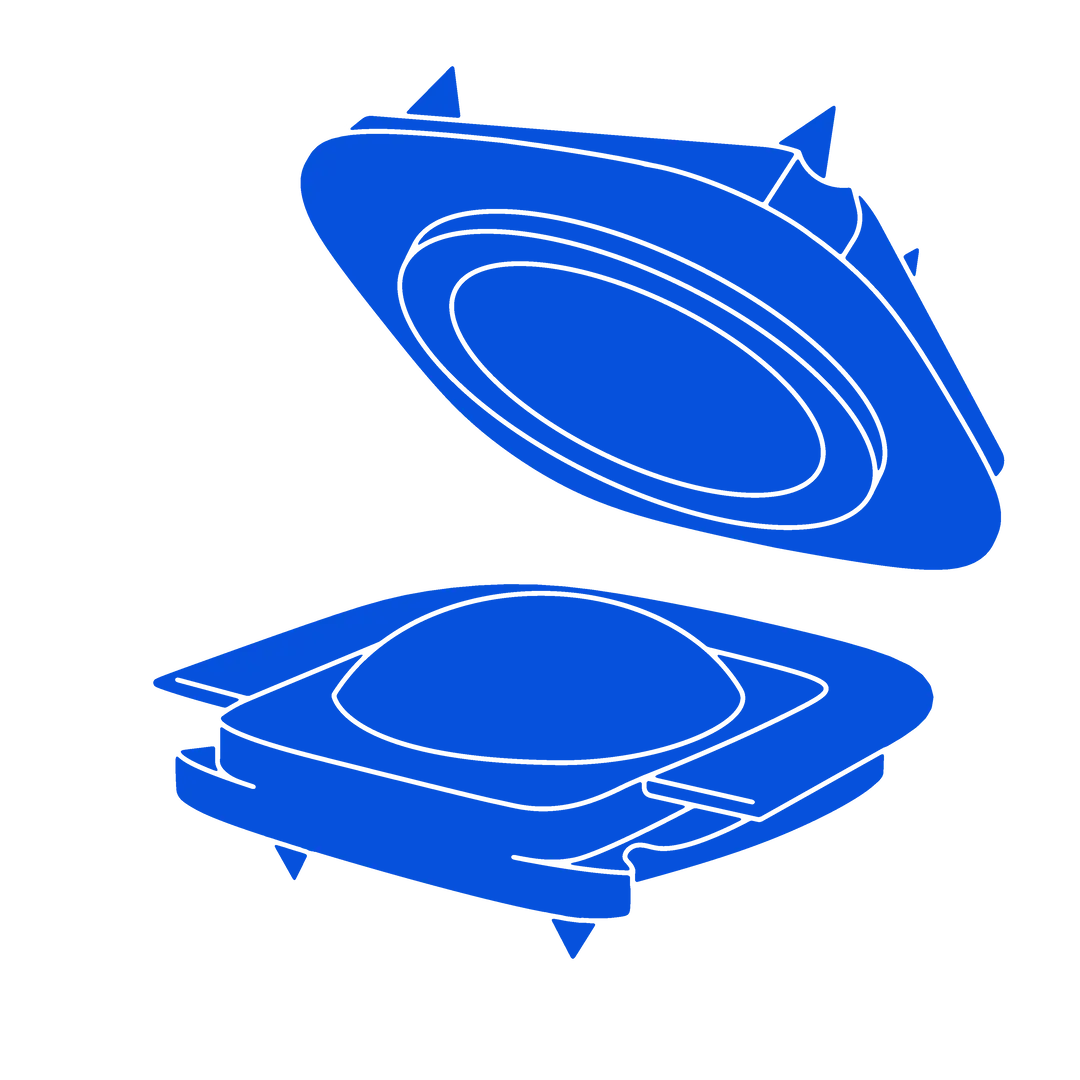
Cervical Disc Replacement (CDR) was developed as an alternative to spinal fusion to restore stability following decompression without limiting motion. Maintaining motion in the neck improves quality of life while minimizing adjacent segment breakdown and other deleterious effects of spinal fusion. CDR consists of placing biologically compatible materials in the disc space that restore and replicate the function of the disc. The artificial disc is attached to the upper and lower vertebrae, providing shear stability to protect the spinal cord. In the neck, most conditions are addressed from the front or anterior approach. Anterior cervical disc instrumentation has proven effective to address a wide variety of cervical indications.
Drs. Thierry Marnay and Karen Beuttner-Janz developed early cervical discs in France and Germany respectively in the 1980s, which were used in thousands of cases and led to development of modern cervical discs. CDRs were first approved by the FDA for use in the United States in 2007. Since that time, many variants have been developed and approved for use at one or two levels, providing improvement in both pain and function, reducing the need for repeat spinal surgery.
Spine conditions often treated with cervical disc replacement include cervical disc herniation, spinal stenosis, and cervical disc degeneration. The surgery typically allows immediate movement of the neck and is routinely carried out as an out-patient procedure.
Several companies offer cervical disc replacement products in the United States, including:
- Centinel Spine – prodisc C
- Medtronic: Prestige LP™
- High Ridge Medical – Mobi-C®
- Globus – SECURE-C®
Lumbar Disc Replacement
The lumbar spine differs from the cervical spine due to markedly increased mechanical forces as well as location of pathology. In the cervical spine, most issues develop in the front of the spinal canal, whereas the low back is more prone to develop instability and nerve compression in the posterior elements. Like Cervical, Drs. Buettner-Janz (Charite) and Marnay (ProDisc) pioneered lumbar disc technology, but indications for isolated disc replacement in the low back are more limited than CDR.
Major pain-generating structures in the low-back include degeneration of the disc, degeneration of the articular joints, nerve compression, mal-alignment, and instability. A patient may present with any combination of these factors. A common cause of chronic low back pain is degeneration of the disc with no abnormality of the other four pain generators, and, in this case, lumbar artificial disc replacements may be well suited to treat the problem.
Surgically, Lumbar Disc Replacement (LDR) is completed through an anterior, lower-abdominal approach. Procedures typically allow for same day discharge or at most one over-night hospital stay, and patients can begin transferring and ambulating immediately post-operatively. Some of the major benefits associated with LDR include retention of motion, faster mobilization, and return to normal activity, including work and sports.
Two lumbar disc replacements are currently FDA approved and marketed in the United States:
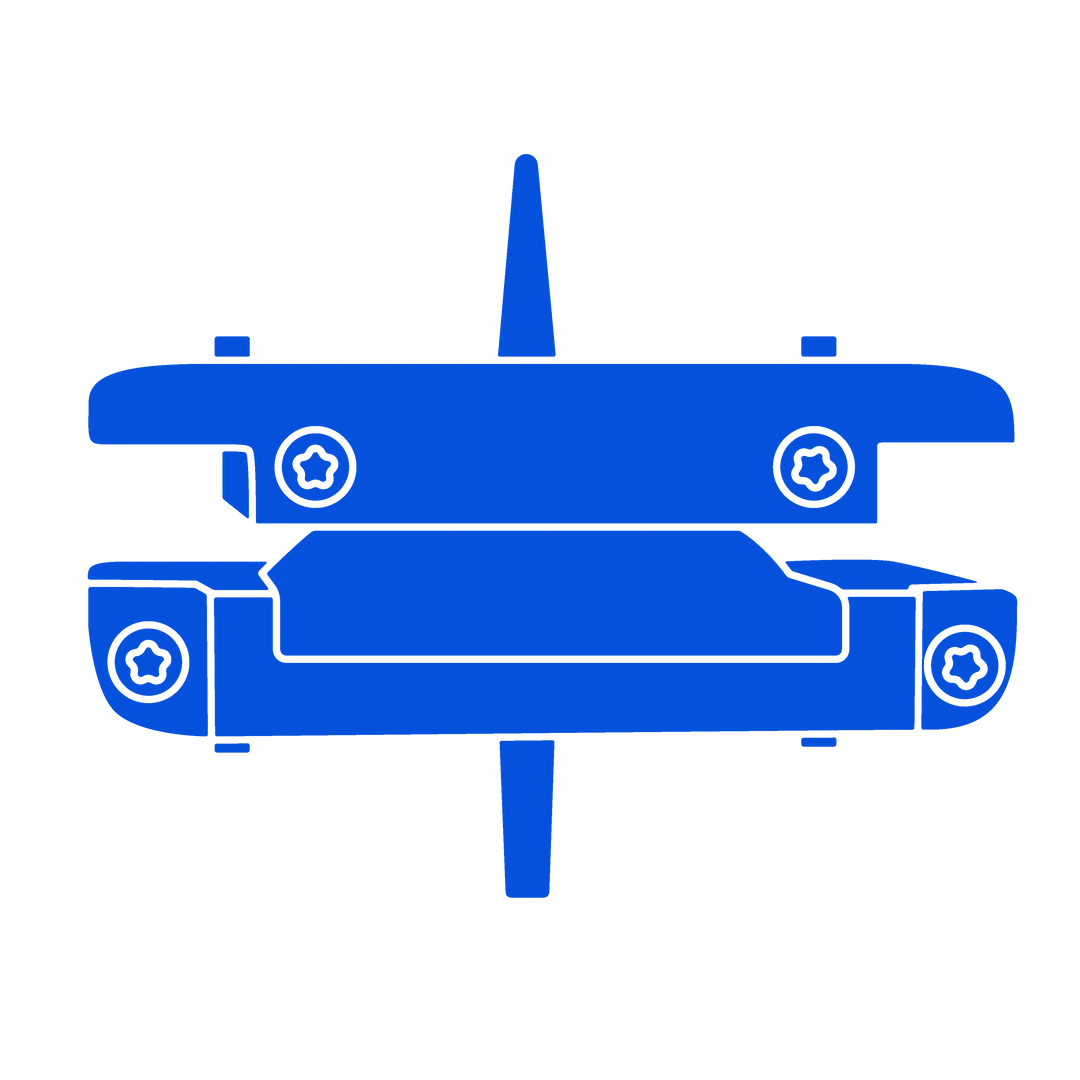
Facet Replacement
Whereas lumbar disc replacements address isolated disc disease where facets and other factors are relatively normal, facet replacements have essentially the opposite indications. Here, the technology is intended to replace the two stabilizing facet joints in the posterior column, while leaving the anterior column and disc intact. The intent is to stabilize the spine without limiting motion. Because the facet joints are removed as part of the procedure, pain associated with facet arthritis is also addressed.
Several anatomical and functional approaches have been proposed for facet replacement. In the early 2000s, Dr. Mark Reiley developed a ball and track system marketed as TFAS, where the functional facets were cemented into the pedicle. At the same time, Dr. Allen Carl imagined an anatomical facet (Globus ACADIA) attached to pedicle screws. Uri Arnin from Impliant (now Premia Spine) developed a pedicle-based, dynamic mechanical control mechanism known as TOPS.
The clinical diagnosis indicated for facet replacement is spinal stenosis with early-stage instability. Benefits include removal of painful arthritic joints, decompression of the nerves, and stabilization of the FSU.
Premia Spine is currently the only company with an approved facet replacement in the United States. The TOPS device was approved for single-level use in 2023.
- Premia Spine – TOPS™
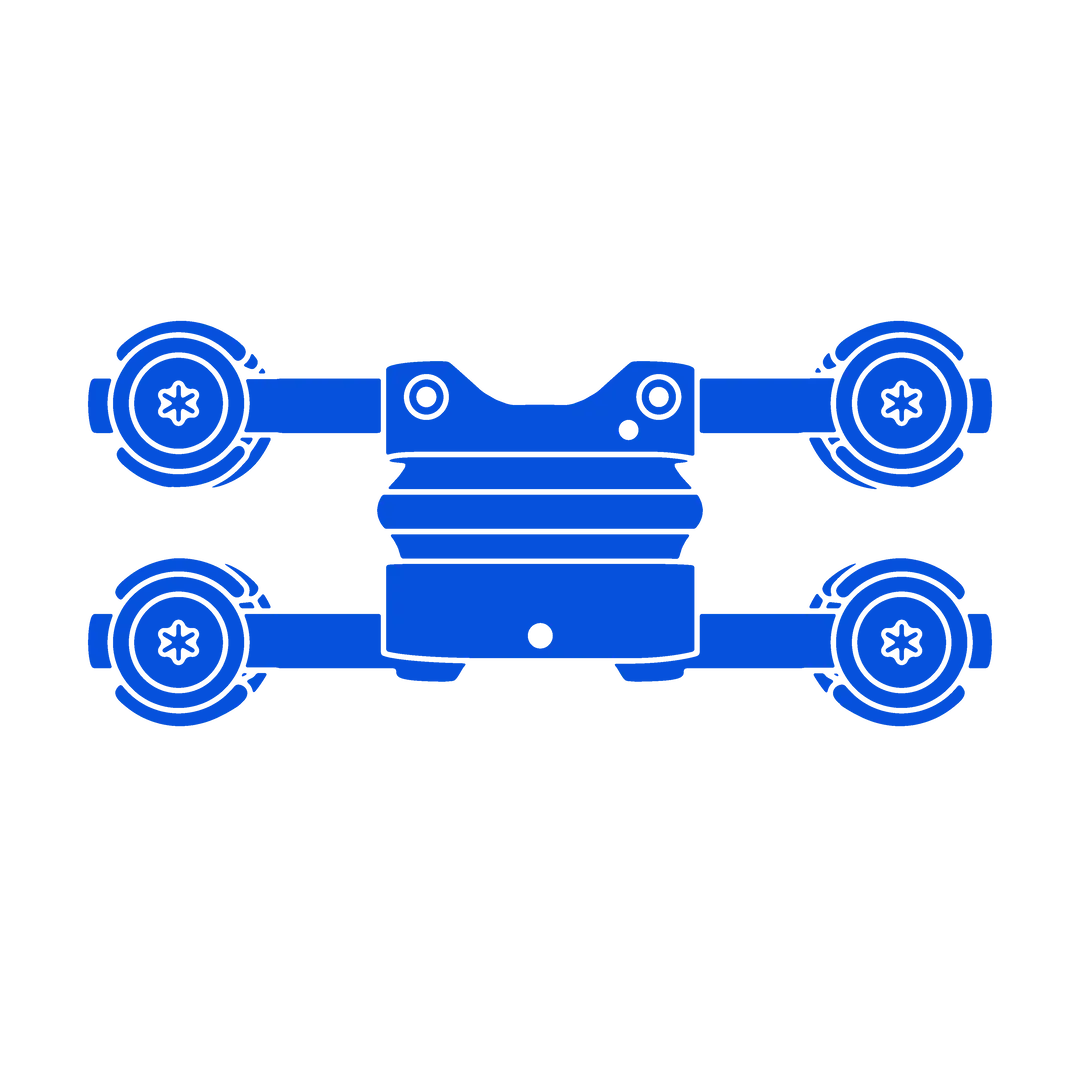
Lumbar Total Joint Replacement
3Spine is currently in the follow-up phase of an ongoing US clinical trial, seeking FDA approval for MOTUS, the first lumbar spine total joint replacement. The procedure combines the benefits of lumbar disc replacement with facet replacement, reproducing the function of the disc and facet joints through a single, posterior approach. Much like cervical disc replacement, the procedure has the promise of addressing a broad range of lumbar pathologies and may replace many common fusion procedures. The procedure was originally developed by Drs. Hodges and Humphreys at Medtronic, who after three clinical pilot studies led the US pivotal trial with 3Spine.
The MOTUS device replaces the function of the disc and facet joints, reestablishing stability after discectomy and broad decompression like a fusion, while retaining natural motion and spinal balance. Like a hip or knee replacement, MOTUS reconstructs all three structures in the functional spinal unit (the disc and two facets), thereby addressing all pain generators including spinal stenosis, facet arthrosis, disc degeneration, spinal instability, and associated muscle spasms. The MOTUS procedure is performed using a posterior midline approach. Pre-operative planning is used to achieve optimal spinal balance through the procedure, allowing patients to comfortably stand, sit, slump, and return to unrestricted activity.
MOTUS is currently in US clinical trials and is not approved for use in the United States.
- 3Spine – MOTUS
Dynamic Tethering
Vertebral Body Tethering (VBT) is a growth modulation technology that provides a non-fusion option for treatment of certain Adolescence Idiopathic Scoliosis (AIS) curves. The Hueter-Volkmann principal is the basis for this treatment, where the convex side of a spinal deformity is tethered to naturally correct the curve through growth. Drs. Lenke, Crawford, Newton and others developed non-fusion growing spine techniques, and a variety of specialize devices are now available in the US for this indication.
Tethering provides the benefit of flexibility while additionally minimizing the need for repeat surgeries. Not all curves respond to tethering. The treating surgeons will determine the flexibility of the curve, the skeletal age of the patient, and predict the amount of growth remaining until they reach skeletal maturity. Adolescences with curves from 20 to 35 degrees are most commonly managed with bracing, whereas patients with curves greater than 65 degrees may require more aggressive reconstruction surgeries such as spinal fusion. The typical AIS patient that qualifies for VBT is skeletally immature with a curve of 35 to 60 degrees and bone maturity of Risser grade 0-1, Sanders stage 2 or 3, with a closed triradiate cartilage growth plate of the hip socket. Only a surgeon who specializes in treatment of spinal deformity is qualified to determine whether an AIS patient is a candidate for VBT. The surgery is performed as an inpatient procedure. No external bracing is required following surgery and the spine maintains mobility throughout life.
Currently there are several companies offering tethering technologies in the United States including:
- Highridge – The Tether™
- Globus– REFLECT®
- Auctus Surgical – VBT
Learn more about Motion Surgery
FAQs